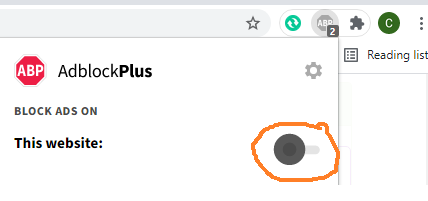
Algorithm depicting clinical approach to hypokalemia. TTKG, transtubular K+ concentration gradient; RTA, renal tubular acidosis. | Chapter 046. Sodium and Water Part 15 Algorithm depicting clinical approach to hypokalemia. TTKG transtubular K concentration gradient RTA renal tubular acidosis. After eliminating decreased intake and intracellular shift as potential causes of hypokalemia examination of the renal response can help to clarify the source of K loss. The appropriate response to K depletion is to excrete 15 mmol d of K in the urine due to increased reabsorption and decreased distal secretion. Hypokalemia with minimal renal K excretion suggests that K was lost via the skin or gastrointestinal tract or that there is a remote history of vomiting or diuretic use. As described above renal K wasting may be due to factors that either increase the K concentration in the CCD or increase the distal flow rate or both . The ECF volume status blood pressure and associated acid-base disorder may help to differentiate the causes of excessive renal K loss. A rapid and simple test designed to evaluate the driving force for net K secretion is the transtubular Kconcentration gradient TTKG . The TTKG is the ratio of the K concentration in the lumen of the CCD K Ccd to that in peritubular capillaries or plasma K p . The validity of this measurement depends on three assumptions 1 few solutes are reabsorbed in the medullary collecting duct MCD 2 K is neither secreted nor reabsorbed in the MCD and 3 the osmolality of the fluid in the terminal CCD is known. Significant reabsorption or secretion of K in the MCD seldom occurs except in profound K depletion or excess respectively. When AVP is acting OSMu OSMP the osmolality in the terminal CCD is the same as that of plasma and the K concentration in the lumen of the distal nephron can be estimated by dividing the urine K concentration K u by the ratio of the urine to plasma osmolality OSMU OSMP Hypokalemia Treatment The therapeutic goals are to correct the K deficit and to minimize ongoing losses. With the exception of periodic paralysis hypokalemia resulting .